How to reach ‘hard-to-reach’ older people for research: The TIBaR model of recruitment
Kammerer, K., Falk K., Herzog A. & Fuchs J. (2019). How to reach ‘hard-to-reach’ older people for research: The TIBaR model of recruitment. Survey Methods: Insights from the Field. Retrieved from https://surveyinsights.org/?p=11822
© the authors 2019. This work is licensed under a Creative Commons Attribution 4.0 International License (CC BY 4.0) 
Abstract
Recruiting older persons with diverse health statuses as participants in research projects is a challenge for health researchers, particularly because persons with health impairments and in socially disadvantaged living conditions are difficult to reach. This article presents a step model for gaining access to older people who are difficult to contact. The step model is based on the literature and a qualitative analysis of documentation, field notes and memos that stem from the recruitment processes of two studies from the German research consortium ‘Autonomy despite multimorbidity in old age’, both of which also included older persons who would qualify as ‘hard-to-reach’. The analysis followed the method of Grounded Theory and aimed to understand the social process of ‘recruitment’. Four steps of the recruitment process were identified that had been applied – intentionally or unintentionally – in both of the projects, i.e., the qualitative as well as the quantitative projects: 1. build up Trust, 2. offer Incentives, 3. identify individual Barriers and 4. be Responsive (TIBaR). The step model provides information for facilitating access to various target groups for qualitative as well as quantitative research designs. However, its implementation requires time, financial resources, flexibility and appropriately qualified staff members.
Keywords
hard to reach populations, older adults, Recruitment, research design
Acknowledgement
The NEIGHBOURHOOD study was funded from 2008 to 2010 by the German Federal Ministry of Education and Research under Grant Numbers 01ET0705 and 01ET0706. The OMAHA study was funded from 2008 to 2010 by the German Federal Ministry of Education and Research under Grant Number 01ET0701. The contents of this publication are solely the responsibility of the authors.
Copyright
© the authors 2019. This work is licensed under a Creative Commons Attribution 4.0 International License (CC BY 4.0) 
Introduction
Due to demographic changes, more people will live longer, and the proportion of older people will rise in the German population as well as worldwide [1, 2]. Older people are more likely than younger people to suffer from multimorbidity, frailty and other syndromes [3, 4]. Older people carry the largest burden of disease and thus make greater use of the health care system [5]. Moreover, with multimorbidity, the probability of needing assistance or care increases [3, 4, 6, 7], and its onset occurs earlier in persons with lower socioeconomic status (SES) than in those with higher SES [3]. Persons in deprived living conditions and with ill health often face special barriers that may hinder them from participating in society in general, as well as in research. Including such groups is therefore a major methodological challenge for empirical research [8-11]. Against this background, these individuals are ‘hard-to-reach’ [12].
Of course, not every older person is hard-to-reach. Instead, healthy older people are often easier to access (because they are no longer working and their time is more flexible) and are more interested in taking part in research than younger, working people [13]. However, people in need of care, severely chronically ill people or cognitively impaired people, as well as their caregivers, are less likely to take part in surveys, examinations or qualitative interviews or focus groups [14]. Quantitative and qualitative studies are generally designed in a way that requires participants to be willing, sufficiently verbally fluent and cognitively able to provide information about their own situation. In some cases, they must be mobile enough to travel to a study centre or to another place outside their immediate living environment or to be able and willing to request a home visit. Specific health-related impediments to participation in such studies like frailty and mental health issues may go along with barriers such as lower educational levels, being a caregiver, and attitudes including distrust or poor perception of health and health research [15-17].
Health research should include older people with diverse health statuses and from various socioeconomic backgrounds to obtain significant and valid results for the whole spectre of this life stage. However, there is broad evidence that some groups participate less often in health research. The Irish Longitudinal Study on Ageing (TILDA) reports a significant correlation for lower socioeconomic status, physical inactivity and smoking with non-participation in health assessments [18]. Participants in the Barcelona Health Study had higher educational levels and family incomes [19]. Controlling for confounders, participation was slightly higher among women than men and lower among the youngest and oldest subjects, with a strong and monotonic trend of increasing participation with increasing educational levels. A 20-year prospective population-based study showed that participants aged 60 years and older by the time of the latest follow-up had higher socioeconomic statuses, lower hospitalization rates due to somatic and psychiatric diseases, better health profiles, and lower mortality rates compared to non-participants [20].
Qualitative studies sometimes explicitly aim to involve ‘hard-to-reach’ groups [21, 22], e.g., older drug users. However, these researchers often struggle to find participants from ‘hard-to-reach’ groups [22]. This situation is even more challenging if disadvantages on the side of the potential participants are intersecting [9]. In conclusion, ‘hard-to-reach’ older people are likely to be implicitly and silently excluded from research if the researchers do not explicitly and actively aim to involve them.
Regarding the other side – the view of the potential participants – quantitative as well as qualitative research on older people’s motivation to participate in studies emphasizes multiple aspects, such as personal interest in the study objective [23, 24] and topic [25], altruism [26], the need for information or access to services [26, 27] and the wish for social contact and support or the hope for personal benefit [28-30].
The major task of recruitment is to overcome barriers and to motivate individuals to participate in health research, particularly older vulnerable people. This is a challenge for qualitative as well as quantitative research designs that are based on different research paradigms and aim at different goals. These differences are also reflected in the recruitment of research participants: Quantitative study designs are mainly based on representative samples to gather quantitative and standardized data that may be analysed by statistical procedures with the aim to test hypotheses. Recruitment is mainly population-based and is contingent upon defined inclusion and exclusion criteria. All study participants should be recruited in the same manner, facilitating the participation for certain subgroups might undermine those principles. In contrast, qualitative research aims at generating theories. The focus lies in subjective and social meanings as well as in the reconstruction of the deep structure of social reality. To do so, many qualitative research designs pursue the goal of theoretical saturation and therefore select maximally contrasting cases [31]. Thus, there is an inherent interest in gaining access to ‘hard-to-reach’ groups. Furthermore, the interpretative research paradigm and methodology as well as the methods of analysis that are accordingly applied to the data require smaller sample sizes than does quantitative research. Therefore, more efforts can be made to obtain access to a single research participant.
Despite those differences in goals and methods, the challenge for both quantitative and qualitative researchers is to access, reach, and recruit participants from ‘hard-to-reach’ groups. Nevertheless, to reach ‘hard-to-reach’ participants, strategies that are more common in qualitative research have also been discussed for quantitative approaches, e.g., the snowball method [21].
Against this background, the article compiles and analyses the insights from a qualitative and a quantitative study regarding access to older, “hard-to-reach” people as well as those with health problems or in disadvantaged living situations. By comparing the recruitment strategies in both studies, it is possible – notwithstanding the differences that result from the distinct underlying research paradigms – to identify similarities in the recruitment process that may be condensed in a theoretical model of recruitment: the TIBaR model.
Data and methods
Description of the NEIGHBOURHOOD and OMAHA studies
The NEIGHBOURHOOD and OMAHA studies were part of the German research consortium ‘Autonomy despite multimorbidity in old age’ (AMA). AMA was funded by the German Federal Ministry of Education and Research as part of a long-term research initiative on ‘Health in Old Age’, along with five other research consortia. The objectives were to identify determinants of autonomy in older and very old people affected by multimorbidity and to develop standardized instruments for the multidimensional analysis of multimorbidity [4].
The study ‘Maintaining autonomy after a fall in socially disadvantaged neighbourhoods’ (NEIGHBOURHOOD) was conducted jointly by IGF e. V. (Institute for Gerontological Research) and the public health research group at WZB (Social Science Research Centre) in Berlin, Germany. The objective of this qualitative study was to describe how community-dwelling senior citizens can maintain autonomy despite their dependency on others for care [32]. The study encompassed a community perspective and considered the positions and attitudes of people aged 60 years and older. To assess the community perspective, 70 qualitative interviews in three different types of neighbourhoods were conducted with representatives of municipal administration services, nursing services, counselling services, or neighbourhood centres. To cover the individual’s perspectives, 60 interviews in the same three neighbourhoods were conducted. All interviews were guideline-based and conducted by trained members of the scientific teams. The sampling design included the recruitment of interview partners from various cultural backgrounds, living situations and caring arrangements. The inclusion criteria were an age of 60 years and older, the ability to communicate about daily life in a comprehensible manner, the need for assistance or care at least five times a week and social disadvantage (operationalized by low income, little formal education, low vocational status and shortcomings in the caring arrangement).
The population-based longitudinal study ‘Operationalizing multimorbidity and autonomy for health services research in ageing populations’ (OMAHA) was a joint study of Charité – Universitaetsmedizin Berlin and the Robert Koch Institute. OMAHA examined multimorbidity within a framework of physical, social and psychological determinants, correlates and consequences [33]. For this study, a multidimensional set of instruments was developed for personal and telephone-based interviews. OMAHA included community-dwelling persons aged 65 years and older with various health statuses, ranging from healthy people to persons with many different chronic conditions. OMAHA collected data from an age- and sex-stratified random sample from the population register in an inner district of Berlin consisting of a variety of urban neighbourhoods, ranging from working-class neighbourhoods with diverse cultural and ethnic groups to neighbourhoods with upper-class residents.
Recruitment for the NEIGHBOURHOOD qualitative study
NEIGHBOURHOOD used a non-representative, theoretical sampling strategy to contact potential interviewees in their particular individual setting via stakeholders in the community who would act as intermediaries.
The NEIGHBOURHOOD study was supported by local authorities, such as the mayor, the head of the welfare and social department, or local social planners, in the three investigated areas: Moabit (a lower-class neighbourhood in the Mitte district of Berlin), Marzahn (a lower-class neighbourhood in the Marzahn-Hellersdorf district of Berlin) and the region around Beeskow in the County Oder-Spree (a rural county in the southeast area of the Brandenburg state). During assessment, in all three areas lived about 8.000 to 10.000 persons aged 65 years and older. The local stakeholders were the administrative staff and managers of social and nursing services, churches, and leisure facilities for senior citizens and local housing associations. They were contacted via letters of information and telephone and asked for cooperation. Cooperation consisted of allowing or initiating their staff to act as intermediaries or giving researchers the opportunity to speak at events for senior citizens, with the aim of introducing the study and call for participation.
The main role of the intermediaries was to ask persons who met the NEIGHBOURHOOD sampling criteria (see above) about their willingness to participate in the study. With the explicitly given consent of interested potential participants, their addresses were forwarded to the research team by the respective intermediaries. The responsible member of the research team then contacted the potential participants via telephone or personally. Participants were free to bring another person (relative, friend) to the first encounter. The aim of the study and the interview was then presented to the potential participant verbally and written in German that was easy to understand. In cases where a potential participant was not fluent in German, a proxy served as a translator. All participants were able to autonomously give their informed consent to participate in the study.
The effort to recruit potential interview partners from the older population required much preliminary work. Recruitment started with exploratory interviews with local authorities and media research on stakeholders, leaders in the community, social networks, and institutions in the field as well as design of the letters of information. Once the local authorities agreed to support the study, stakeholders in the field were contacted via telephone, in some cases also personally, to help find potential interview partners. The recruitment required approximately 90 to 100 hours within a 3-month term; thus, 20 to 30 interviewees needed to be recruited in each of the three investigated neighbourhoods.
Recruitment for the OMAHA quantitative study
In the Berlin OMAHA cohort, persons aged 65 years and older were recruited from a large age- and sex-stratified random sample drawn from the population registry in the inner-city district of Berlin-Mitte. People living in nursing homes were not excluded from the sample, but recruitment was not successful [34]. The ‘Mitte’ district consists of a variety of urban neighbourhoods, ranging from working-class neighbourhoods with diverse cultural and ethnic groups to neighbourhoods with upper-class residents. In 2008, 47,000 inhabitants aged 65 years and older lived in the district [35].
The recruitment process started with a letter of invitation including a brief description of the study, a prepaid self-addressed envelope, and a sheet for sending back the potential participant’s phone number and best times to be contacted by our study nurses. The respondents were called within two weeks, and appointments were made as soon as possible, mainly during the following three weeks. The participants received a confirmation letter with the date and direction. Those who did not respond within four weeks were contacted via three different recruitment strategies: (a) personal visits, (b) telephone calls, or (c) mailed reminder letters. The entire recruitment process took six months. Out of 1308 eligible persons, 299 (22.9%) participated [34]. The interviews and examinations were conducted by three experienced study nurses who were initially trained and continuously supervised during the data collection.
Comparison of the recruitment strategies
Within the research consortium, the NEIGHBOURHOOD and OMAHA teams worked closely together in an interdisciplinary manner. Part of this approach was a project-overarching working group in which the researchers discussed their respective strategies for recruiting participants from ‘hard-to-reach’ groups of older persons. This process was continued by the authors after the formal ending of the research projects with the aim of systematically analysing the experiences of both teams during the recruitment process. The research questions that were applied to the accessible material were a) how to successfully gain access to ‘hard-to-reach’ older persons and b) the overlapping strategies and overarching efforts that could be identified in the recruitment processes of both the qualitative and the quantitative studies.
As a basis for their analysis, the authors used documentation, field notes and memos that they had produced in planning, conducting and reflecting on the recruitment process in their respective teams. The analysis of the documents followed the Grounded Theory approach [36] and aimed at understanding the social process of “recruitment”. The material of both projects was initially coded [37],followed by focused coding, whereby the most significant and frequent codes were selected, condensed and labelled (e.g., the initial codes “contact reliable gatekeeper” “encourage personal and confidential contact” into the focused code “building up trust”). In comparing the processes of recruitment from both studies, they were condensed to four comprehensive focused codes associated with strategies that had intentionally or unintentionally been applied in both of the projects.
Results
Although there were differences in the study designs, parallels in the recruitment proceedings for the OMAHA and NEIGHBOURHOOD studies could be identified. In both studies, the contact with potential interviewees was designed with the intention of building a positive relationship and trust. Various stimuli were explicitly or implicitly offered to promote participation: the incentives. Both studies were designed to learn more about a participant’s personal situation to identify individual barriers. Ultimately, responsiveness was another important strategy to overcome barriers to participation.
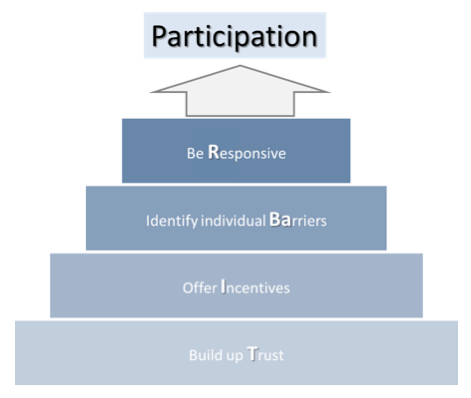
Finally, four central steps were identified and labelled the TIBaR model of recruitment:
- Build up Trust,
- Offer Incentives,
- Identify individual Barriers and
- Be Responsive.
In the following sections, we provide detailed information and examples of the four steps from the NEIGHBOURHOOD and OMAHA studies (see also Table 1).
Build up trust
In both studies, building up trust and confidence was the crucial first step in communicating to multipliers, gatekeepers and potential study participants that these could be important and significant research projects for them. This was particularly necessary because some participants and facilitators reported negative experiences with similar requests or had experienced fake attempts. The building of trust can be achieved by various partially complementary measures.
Building trust via accessible informational materials
In both studies, informational materials for potential study participants were provided in easily understandable language and large font size. The OMAHA study included a leaflet with basic information on the study, which was available in the languages of the largest population groups in the district of Mitte (German, Turkish, Russian, Arabic, Serbian, Croatian, Polish and English), and a free hot-line telephone number.
Building trust via trustworthy institutions
As a study by the Robert Koch Institute and the Charité-Universitaetsmedizin Berlin, OMAHA was able to highlight two well-known and trusted institutions in Berlin, both of which have been funded by the sponsoring Federal Ministry. These institutions were showcased using the logos and instructions in the text on all informational materials and cover letters.
Building trust via gatekeepers and multipliers
In the NEIGHBORHOOD study, access was provided through persons who had the confidence of local actors, such as mayors or deputies, and key persons in welfare organizations or care services. A top-down strategy was applied, which means that persons at higher organizational levels were addressed first. The support of mediators on higher hierarchical levels helped build the trust of other stakeholders and, consecutively, of potential study participants.
Building trust via personal contact, transparent communication and careful data protection
Both research projects provided informed consent and data protection according to the German regulations for data protection. As in OMAHA, some medical tests were also performed; additionally, information on the local ethics committee’s approval of the study was provided.
Offer incentives
The results of both studies underline the importance of various incentives. These incentives may be material (e.g., expense allowance) or immaterial (e.g., opportunity to express oneself). Some of these incentives have been offered explicitly and some implicitly by being held out in prospect.
In NEIGHBOURHOOD, one important incentive to participate was the opportunity to reveal one’s own living situation or priorities and opinions on the subject of long-term care and to organize one’s daily living in the respective local area. The interviewees could address personal concerns that were not directly related to the study’s purpose (called participatory incentive). Further incentives were the opportunity to enjoy company (social incentive). All these incentives were presented indirectly and offered implicitly in the preliminary talks. Although these offers have not been made explicitly, they resulted in strong incentives.
The OMAHA letter of invitation indicated that there was an opportunity to talk about one’s own situation. Additionally, the motive of contributing to the research and improving the situations of older people was an incentive for both studies (altruistic incentive).
Another motive for the participants in both studies was the need for information, which was met by providing contact details for centres offering information and advice, e.g., care counselling centres.
In NEIGHBOURHOOD, there was an incentive for intermediaries to be informed about research results and thus obtain information about their district or their clientele. Therefore, the research results were referred to the local authorities and presented at several public events in each of the three investigated neighbourhoods, e.g., in front of senior citizens’ councils.
In OMAHA, the participants were offered written feedback on the results of their physical function assessment (e.g., cognitive abilities, blood pressure) after participation. The interest in these results was very high (informational incentive).
OMAHA offered a material incentive in the form of an allowance of 10 Euros. The reactions of participants, particularly those with low financial resources, showed that the financial incentive was important for them (monetary incentive).
Identify individual barriers
Even if the participants’ trust is gained and they acknowledge the incentives, participation may still be hampered by individual and situational obstacles. It is important to be aware of such potential impediments in the course of the recruitment process. Possible means to do so are to retrieve literature about the difficulties of specific sub-groups or to organize preliminary interchanges with intermediaries and potential participants, as part of the telephone contacts or during the presentation of the aims of the study on meetings or events.
In both studies, the major barriers to participation were mobility limitations of various kinds, language difficulties and responsibilities for the care of relatives.
In NEIGHBOURHOOD, language proficiency and time frames were identified as possible hindrances as well as individual worries or needs; for example, a person who did not want to be alone with an interviewer wanted only one (and not two) interviewer or preferred a male or female interviewer (needs regarding communication).
The inclination to take part in the study also depended on the general workload (e.g., of civil engagement or caring for oneself and/or others) and time constraints that some older people experience (availability with regard to time).
In OMAHA, critical life events such as the death of a close family member or a friend and acute health problems (e.g., reduced mobility, acute infectious disease) may have led to a delay in participation. With the invitation letter, potential participants received a telephone number and email address so they could phone or mail and inform the study centre about difficulties such as current complaints or critical life events (for example, recent death of a spouse) (individual worries or needs ).
Additionally, functional limitations or mobility restrictions turned out to be potential barriers to participation. Furthermore, potential participants’ residence (residential home, community dwelling) and personal health situation, including impairments and handicaps or those of close relatives, were also important to consider.
Thus, for both studies, one can assert an inbuilt openness to information on possible hindrances originating from the specific situation prevailing for a potential participant. To identify these barriers means to acknowledge their existence and to look for possible solutions, leading to the next step: being responsive.
Be responsive
Considering the personal situations of potential study participants, flexibility and the use of appropriate resources and measures are central to overcoming barriers, as mentioned above. To foster older persons’ participation, suitable, needs-based offers that respect the autonomy and wishes of the individuals are essential, keeping in mind that not every obstacle is relevant for every participant. One barrier, which is frequently termed ‘temporal restrictions’, can be addressed with the flexible scheduling of interviews, which was offered in both projects. Barriers such as a high need for security were faced through offering a choice of interview location and the presence of a trusted person. Limited mobility was compensated through a mobility assistance service and accessible facilities. Insufficient knowledge of German was overcome through the use of interpreters. For people with low income, the reimbursement of travel expenses proved to be helpful.
Based on the experience from both studies, we thus identified adequate strategies to recruit heterogeneous samples of older persons. The suggested recruitment strategy provides a variety of possible measures that can be applied simultaneously for the various needs and interests of ‘hard-to-reach’ older participants.
The conjoint and divergent implementations of the four aspects of both studies are illustrated in Table 1.
Table 1: Overview of the aspects considered during recruitment in both studies
| Aspects considered | NEIGHBOUR-HOOD | OMAHA | |
| Build up trust | Providing letter of information and informational materials about the study in easily understandable language and large font size | + | + |
| Referring to (reliable) authorities | + | + | |
| Information of (potential) gatekeepers | + | + | |
| Contact of potential participants via trusted intermediaries | + | – | |
| Personal attendance of researchers in the field (opportunity for personal contact) | + | + | |
| Offer incentives | Participatory incentives (forum for participants’ opinions) | + | – |
| Social incentives (opportunity to enjoy company) | + | – | |
| Emotional incentives (having someone to talk to about health) | + | + | |
| Altruistic incentives (contribution to research or to the improvement of the situation of senior citizens in one’s own community | + | + | |
| Informational incentive (e.g., feedback about health status, such as a standardized letter summarizing relevant study results) | + | + | |
| Small monetary incentives, refunding travel expenses | – | + | |
| Needs regarding communication (language proficiency) | + | + | |
| Identify individual barriers | Availability with regard to time (caring duties, civil engagement or similar activities) | + | + |
| Individual worries or needs (illness, loss of a close person) | + | + | |
| Functional limitations | + | + | |
| Mobility restrictions | + | + | |
| Place of living (community dwelling, residential care) | – | + | |
| Flexibility in location for interview (home visit or study centre) | + | + | |
| Be responsive | Flexibility in scheduling with choice of date and time (morning, afternoon, evening) | + | + |
| Choose study centre in a well-known university hospital | – | + | |
| Allow presence of familiar third persons during the interview | + | + | |
| Offer interpreter if necessary | + | + | |
| Reimburse travel expenses | – | + |
The TIBaR model of recruitment
As shown above, the underlying structure of the analysed recruitment processes encompasses four consecutive steps that may be generalized in the TIBaR model of recruitment of ‘hard-to-reach’ groups: building up trust, offering and providing incentives, learning about and identifying specific individual situations and being responsive to overcoming frequent barriers and help potential participants feel safe and comfortable.
Moreover, in analysing the recruitment process, we found a) that a sequential logic underlies the recruitment process and b) that a combination of these steps is necessary to process the later steps based on the results of the earlier steps (“additive strategy”). Figure 1 shows the four steps of the recruitment process.
Figure 1: Common elements of the recruitment process: the TIBaR model
Discussion
We presented a step model for accessing ‘hard-to-reach’ groups, which is an outline of how to improve age-specific recruitment strategies. These strategies are needed to increase participation rates in future investigations [38-40].
As a limitation of the model could be considered that it was developed on the basis of the recruitment processes of only two studies. In accordance with the logic of maximal contrasting cases, these studies represented maximal contrasting cases by pertaining to different research paradigms. To meet this limitation we further complemented the process analysis by an extensive literature search, that has contributed to the plausibility of the model: A recent review showed that fewer studies and fewer successful strategies exist for improving the participation of older adults in research studies than for improving research study participation in the wider population [41].
Some of the strategies and barriers developed in this article are referred to in several other studies or literature reviews, albeit in a less systematic way. In a clinical trial, McHenry, Insel et al. [42] identified four strategies as important for recruitment and retention, namely, accessing an appropriate population, communicating and building trust, providing comfort and security, and expressing gratitude, giving valuable examples mainly for the retention of older people. Hughson, Woodward-Kron et al. [40] recognized barriers to the participation of culturally and linguistically diverse older people in clinical research: mistrust, communication barriers, cultural barriers, economic and time constraints, mobility and health issues as well as opportunity barriers.
Promising strategies for building trust are suggested in the literature: forming community partnerships [9], identifying the ‘gatekeepers’ in the setting and building trust with stakeholders [43], establishing a partnership with staff that participants know and trust [44], or enlist the social support of caregivers, family, friends and the medical community, particularly general practitioners [45]. In sum, stakeholders on different levels are known to play important roles in enabling access to targeted older persons. The importance of using suitable information materials is underlined by McHenry, Insel et al. [42], who understand communication as a trust-building measure and invest effort in, for example, designing informational brochures for participants and stakeholders. Communication barriers include the complexity of written documents, language/literacy issues and lack of perceived benefit [40].
The existing literature also makes many references to the need to offer incentives for participation. It was shown that it is important to convey to participants the benefits they might receive through participation and to maximize the benefits to them and the convenience of participating [43]. Furthermore, incentives might be immaterial or material. Baczynska, Shaw et al. [46] note that personal motives for participation (potential health benefit for oneself and one’s family; curiosity; comparing one’s own fitness to others’ fitness; socializing) as well as altruistic motives (benefit to other people; belief in the importance of research) are important.
Identifying barriers is referred to in the literature as understanding the culture of the research setting [43] and considering poor health and mobility problems [44].
The final step to successful recruitment is being responsive. Several studies note that being flexible about the time and place of the study [9] [44] [47], providing comfort and security, including home visits [47], minimizing the burden of the study [43], acknowledging extended timeframes, and planning for higher resourcing costs [9] are important measures in the recruitment process.
What is still lacking is a comprehensive model that systematizes the existing knowledge on necessary steps according to their inner logic. The innovation of the step model lies in the systematization of the necessary steps and the identification of its sequential and additive character. The strength of the TIBaR model is that it unifies very different strategies and summarizes them in abstract, generalizing terms so that they can be applied and aligned to different target groups and research paradigms. Thus, the model can easily be transferred and adopted to other ‘hard-to-reach’ groups.
Additionally, in participatory approaches that can increase the willingness to participate, the four steps are important. It would be interesting to compare the extent to which the measures vary at the different steps. Thus, intermediaries or peers may play a role in trust building, and the incentives to join the research may be different.
The TIBaR model of recruitment will be useful for the planning of individualized strategies tailored to special target groups, both with qualitative and quantitative research designs and regardless of the size of the studied population. Even in huge studies, individualized strategies are applicable, for example, by consulting experts who concentrate on special subgroups of the sample. The concrete application of the model in qualitative and quantitative research designs clearly will differ. For example, in quantitative research designs, there are other means used to build up trust than those used in qualitative research designs. Additionally, the incentives vary, and the possibilities of understanding barriers may differ.
Nevertheless, it is possible to design strategies for both paradigms and to increase participation. Most likely, the usage of such strategies is already more common in qualitative research than in quantitative research. One reason for this may be that quantitative research usually should apply the same conditions for all participants. That may be a contradiction to designing a different recruitment for diverse groups.
The implementation of the TIBaR model for ‘hard-to-reach’ groups requires a high degree of flexibility, increases the complexity of recruitment, and needs more extensive effort and resources. On the other hand, if a middle-class bias can be reduced and the participation rates of socially disadvantaged people increase, so does the meaningfulness of the studies.
It is especially worthwhile and an advantage of the TIBaR model to see and implement the process of recruitment as a learning system. Various small- and large-scale recruitment strategies can be designed to incorporate openness towards learning and capability for adaption. It is not only from the literature but also later on during the research process – in the pre-test and during recruitment – that research teams will recognize which groups are hard-to-reach. It is a matter of pragmatism to identify these difficulties and modify the strategies for ‘hard-to-reach’ groups by making more and different efforts or including other authorities and/or trusted multipliers in the research process. It is also a way to shift the view from possible complaints about ‘hard-to-reach’ groups to responsibility for high-quality research design.
A major issue in reaching the ‘hard-to-reach’ is the resources needed for high flexibility. McHenry, Insel et al. [42] underline that costs for recruiting and retaining individuals from older and underserved groups are high and must be anticipated. The time, staff and ‘hardware’ (electronic devices, flyers, and leaflets) needed require adequate and sufficient financing.
Additionally, non-material resources are essential, such as the capacity for planning and organizing and the recruitment of intensively qualified staff with soft skills such as language proficiency, flexibility and the ability to find the ‘right tone’ in communicating with participants from diverse socioeconomic milieus and strata.
In planning and funding research projects, it is important to carefully consider the target group and the necessary steps for recruitment as well as the required resources. Every research project must clarify in advance whether adaptations to the recruitment process are possible and how many dropouts are tolerable.
In this context, carefully applying all the steps presented in the step model – building trust, offering adequate incentives, learning about and identifying actual personal situations and being responsive by providing facilitating factors – should contribute to making participation in gerontological and health research more accessible and attractive for ‘hard-to-reach’ groups of older people.
Finally, further research is needed, e.g., in terms of systematic comparison between study variations and recruitment outcomes using the step model or in terms of evaluations by the participants.
References
- Federal Statistical Office of Germany, Germany’s population by 2060. Results of the 13th coordinated population projection, destatis, Editor. 2015: Wiesbaden.
- World Health Organization. WHO facts about ageing Aug 03, 2018]; Available from: http://www.who.int/ageing/about/facts/en/.
- Barnett, K., S.W. Mercer, M. Norbury, G. Watt, S. Wyke and B. Guthrie, Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet, 2012. 380(9836): p. 37-43.
- Scheidt-Nave, C., S. Richter, J. Fuchs and A. Kuhlmey, [Challenges to health research for aging populations using the example of “multimorbidity”]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz, 2010. 53(5): p. 441-50.
- Goodbrand, J.A. and M.E. McMurdo, Overcoming obstacles to clinical research in older people. Maturitas, 2013. 76(4): p. 294-5.
- Marengoni, A., S. Angleman, R. Melis, et al., Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev, 2011. 10(4): p. 430-9.
- Salive, M.E., Multimorbidity in older adults. Epidemiol Rev, 2013. 35: p. 75-83.
- Aglipay, M., J.L. Wylie and A.M. Jolly, Health research among hard-to-reach people: six degrees of sampling. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 2015. 187(15): p. 1145-1149.
- Bonevski, B., M. Randell, C. Paul, et al., Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Medical Research Methodology, 2014. 14: p. 42-42.
- Gao, L., E. Green, L.E. Barnes, et al., Changing non-participation in epidemiological studies of older people: evidence from the Cognitive Function and Ageing Study I and II. Age and ageing, 2015. 44(5): p. 867-873.
- Kelfve, S., M. Thorslund and C. Lennartsson, Sampling and non-response bias on health-outcomes in surveys of the oldest old. European Journal of Ageing, 2013. 10(3): p. 237-245.
- Sydor, A., Conducting research into hidden or hard-to-reach populations. Nurse Res, 2013. 20(3): p. 33-7.
- Golomb, B.A., V.T. Chan, M.A. Evans, S. Koperski, H.L. White and M.H. Criqui, The older the better: are elderly study participants more non-representative? A cross-sectional analysis of clinical trial and observational study samples. BMJ Open, 2012. 2(6): p. e000833.
- Mody, L., D.K. Miller, J.M. McGloin, et al., Recruitment and retention of older adults in aging research. J Am Geriatr Soc, 2008. 56(12): p. 2340-8.
- Crawford Shearer, N.B., J.D. Fleury and M. Belyea, An innovative approach to recruiting homebound older adults. Res Gerontol Nurs, 2010. 3(1): p. 11-8.
- Dibartolo, M.C. and S. McCrone, Recruitment of rural community-dwelling older adults: barriers, challenges, and strategies. Aging Ment Health, 2003. 7(2): p. 75-82.
- Samelson, E.J., J.L. Kelsey, D.P. Kiel, et al., Issues in conducting epidemiologic research among elders: lessons from the MOBILIZE Boston Study. Am J Epidemiol, 2008. 168(12): p. 1444-51.
- Kearney, P.M., H. Cronin, C. O’Regan, Y. Kamiya, B.J. Whelan and R.A. Kenny, Comparison of centre and home-based health assessments: early experience from the Irish Longitudinal Study on Ageing (TILDA). Age Ageing, 2011. 40(1): p. 85-90.
- Porta, M., M. Gasull, E. Puigdomenech, et al., Sociodemographic factors influencing participation in the Barcelona Health Survey study on serum concentrations of persistent organic pollutants. Chemosphere, 2009. 76(2): p. 216-25.
- Drivsholm, T., L.F. Eplov, M. Davidsen, et al., Representativeness in population-based studies: a detailed description of non-response in a Danish cohort study. Scand J Public Health, 2006. 34(6): p. 623-31.
- Atkinson, R., Flint, J, Accessing Hidden and Hard-to-reach Populations: Snowball Research Strategies. Social Research Update, 2001. 33.
- Waters, J., Snowball sampling: a cautionary tale involving a study of older drug users AU – Waters, Jaime. International Journal of Social Research Methodology, 2015. 18(4): p. 367-380.
- Herzog, A.R. and R.A. Kulka, Telephone and Mail Surveys with Older Populations: A Methodological Overview., in Special Research Methods for Gerontology, M.P. Lawton and R.A. Herzog, Editors. 1989, Baywood Publishing: Amityville. p. 69-89.
- Gemmill, R., A.C. Williams, L. Cooke and M. Grant, Challenges and strategies for recruitment and retention of vulnerable research participants: promoting the benefits of participation. Appl Nurs Res, 2012. 25(2): p. 101-7.
- Groves, R.M., S. Presser and S. Dipko, The Role of Topic Interest in Survey Participation Decisions. Public Opinion Quarterly, 2004. 68(1): p. 2-31.
- Gysels, M., C. Shipman and I.J. Higginson, “I will do it if it will help others:” motivations among patients taking part in qualitative studies in palliative care. J Pain Symptom Manage, 2008. 35(4): p. 347-55.
- Townsend, A. and S.M. Cox, Accessing health services through the back door: a qualitative interview study investigating reasons why people participate in health research in Canada. BMC Medical Ethics, 2013. 14(1): p. 40.
- Connell, C.M., R.M. Davies, A.M. Rosenberg and E.B. Fisher, Jr., Retiree’s perceived incentives and barriers to participation in health promotion activities. Health Educ Res, 1988. 3(3): p. 325-330.
- Newburg, S.M., A.E. Holland and L.A. Pearce, Motivation of subjects to participate in a research trial. Appl Nurs Res, 1992. 5(2): p. 89-93.
- Williams, B., V. Entwistle, G. Haddow and M. Wells, Promoting research participation: why not advertise altruism? Soc Sci Med, 2008. 66(7): p. 1451-6.
- Strübing, J., Grounded Theory: Methodische und methodologische Grundlagen, in Praxis Grounded Theory: Theoriegenerierendes empirisches Forschen in medienbezogenen Lebenswelten. Ein Lehr- und Arbeitsbuch, C. Pentzold, A. Bischof, and N. Heise, Editors. 2018, Springer Fachmedien Wiesbaden: Wiesbaden. p. 27-52.
- Kammerer, K., K. Falk, J. Heusinger and S. Kümpers, Selbstbestimmung bei Pflegebedürftigkeit: Drei Fallbeispiele zu individuellen und sozialräumlichen Ressourcen älterer Menschen [Self-determination of elderly persons with care needs. Three case reports on individual and environmental resources of elderly persons]. Zeitschrift für Gerontologie und Geriatrie, 2012. 45(7): p. 624-629.
- Holzhausen, M., J. Fuchs, M. Busch, et al., Operationalizing multimorbidity and autonomy for health services research in aging populations–the OMAHA study. BMC Health Serv Res, 2011. 11: p. 47.
- Gaertner, B., I. Seitz, J. Fuchs, et al., Baseline participation in a health examination survey of the population 65 years and older: who is missed and why? BMC Geriatr, 2016. 16: p. 21.
- Statistical Office for Berlin-Brandenburg. Statistics for the City of Berlin. Population 2008. Available from: https://www.statistik-berlin-brandenburg.de.
- Strauss, A. and J. Corbin, Grounded Theory: Grundlagen Qualitativer Sozialforschung [Grounded theory. Basics of Qualitative Research]. 1996, Weinheim: Beltz
- Charmaz, K., Constructing Grounded Theory. A Practical Guide through Qualitative Analysis. 2006, London, California, New Delhi: SAGE Publications.
- Green, E., H. Bennett, C. Brayne and F.E. Matthews, Exploring patterns of response across the lifespan: the Cambridge Centre for Ageing and Neuroscience (Cam-CAN) study. BMC Public Health, 2018. 18(1): p. 760.
- UyBico, S.J., S. Pavel and C.P. Gross, Recruiting vulnerable populations into research: a systematic review of recruitment interventions. J Gen Intern Med, 2007. 22(6): p. 852-63.
- Hughson, J.A., R. Woodward-Kron, A. Parker, et al., A review of approaches to improve participation of culturally and linguistically diverse populations in clinical trials. Trials, 2016. 17(1): p. 263.
- Lacey, R.J., R. Wilkie, G. Wynne-Jones, J.L. Jordan, E. Wersocki and J. McBeth, Evidence for strategies that improve recruitment and retention of adults aged 65 years and over in randomised trials and observational studies: a systematic review. Age Ageing, 2017. 46(6): p. 895-903.
- McHenry, J.C., K.C. Insel, G.O. Einstein, A.N. Vidrine, K.M. Koerner and D.G. Morrow, Recruitment of Older Adults: Success May Be in the Details. Gerontologist, 2015. 55(5): p. 845-53.
- Anuruang, S., P.M. Davidson, D. Jackson and L. Hickman, Strategies to enhance recruitment of rural-dwelling older people into community-based trials. Nurse Res, 2015. 23(1): p. 40-3.
- Provencher, V., W.B. Mortenson, L. Tanguay-Garneau, K. Belanger and M. Dagenais, Challenges and strategies pertaining to recruitment and retention of frail elderly in research studies: a systematic review. Arch Gerontol Geriatr, 2014. 59(1): p. 18-24.
- Cusack, S., P.W. O’Toole and E. consortium, Challenges and implications for biomedical research and intervention studies in older populations: insights from the ELDERMET study. Gerontology, 2013. 59(2): p. 114-21.
- Baczynska, A.M., S.C. Shaw, H.P. Patel, A.A. Sayer and H.C. Roberts, Learning from older peoples’ reasons for participating in demanding, intensive epidemiological studies: a qualitative study. BMC Med Res Methodol, 2017. 17(1): p. 167.
- Liljas, A.E.M., K. Walters, A. Jovicic, et al., Strategies to improve engagement of ‘hard to reach’ older people in research on health promotion: a systematic review. BMC Public Health, 2017. 17(1): p. 349.