The Impact of Nurse Continuity on Biosocial Survey Participation
Cernat, A. & Sakshaug, J. W. (2020). The Impact of Nurse Continuity on Biosocial Survey Participation in Survey Methods: Insights from the Field. Retrieved from https://surveyinsights.org/?p=13222
© the authors 2020. This work is licensed under a Creative Commons Attribution 4.0 International License (CC BY 4.0) 
Abstract
Biological measurements (or biomeasures) are increasingly being collected in large longitudinal biosocial surveys, enabling researchers to exploit the advantages of social science data with objective health measures to better understand how health and social behaviour interact over time. However, not all survey respondents are willing to take part in the biomeasure component of biosocial surveys, even when the measures are administered by certified medical professionals, such as nurses. Thus, understanding factors which affect participation in biomeasure collection is essential for making valid biosocial inferences about the population. Previous research has shown that interviewer continuity can be useful for optimizing longitudinal survey participation, but it is yet unknown if nurse continuity impacts the likelihood of participation in biomeasure collection. We investigated the impact of nurse continuity on nonresponse to biomeasure collection in waves 4 and 6 of the English Longitudinal Study of Ageing (ELSA). Using cross-classified multilevel models, we find that switching nurses between waves does not negatively impact participation in biomeasure collection, and sometimes can be beneficial, particularly for previous wave nonrespondents. The practical implication is that biosocial surveys may not need to employ strict nurse continuity protocols to maximize participation in subsequent waves of biomeasure data collection.
Keywords
biological data, biosocial surveys, longitudinal study, Nonresponse, nurses
Copyright
© the authors 2020. This work is licensed under a Creative Commons Attribution 4.0 International License (CC BY 4.0) 
1 Introduction
Physical and biological measurements collected in representative social surveys, also known as “biosocial surveys,” are in high demand (Beebe, 2007; Sakshaug et al., 2015). Biosocial surveys are known for their collection of traditional interview data, covering a variety of social and behavioural topics, coupled with the collection of objective health measures (or “biomeasures”) such as anthropometric measurements (e.g. height, weight, waist circumference), physical performance measurements (e.g. lung flow, grip strength), and biological samples (e.g. blood, urine). The combination of social and biomeasure data enable researchers to answer important and complex research questions uncovering the interrelationships between physiological processes and social- and health-related outcomes (National Research Council, 2010, 2008, 2001). Several high-profile biosocial surveys collect longitudinal data on population representative samples, including the US Health and Retirement Study (HRS), the UK English Longitudinal Study of Aging (ELSA), the UK Household Longitudinal Study (UKHLS), also known as Understanding Society, and the Survey of Health, Aging, and Retirement in Europe (SHARE). Data from these biosocial surveys and others have been used to illuminate the interplay between one’s physiological status and their socio-economic status (Das, 2013; Geronimus et al., 2015; Yang et al., 2017), social relationships and behaviors (Das, 2019; Das and Nairn, 2014; Yang et al., 2016), and environmental conditions (Holmes and Marcelli, 2012; Honda et al., 2017; Ludwig et al., 2011).
Considering the potentially sensitive and invasive nature of some biomeasures, particularly venous blood collection, it is often necessary to employ certified medical professionals to carry out the biomeasure component of a biosocial survey. This is especially common in the UK where both the ELSA and UKHLS employ nurses to visit respondents in their homes after the main interview has taken place (McFall et al., 2012; Steptoe et al., 2013). Deploying nurses to administer the biomeasure component over multiple waves of longitudinal data collection raises methodological issues, particularly the issue of nonresponse. Achieving high response rates to the biomeasure collection is crucial to the success and utility of biosocial survey data as it minimizes the risk of nonresponse bias in estimates derived from these data.
Given the existing literature showing the impact of interviewers on participation and measurement (West and Blom, 2017), it is essential to understand how the new actor in biosocial research, the nurse, can impact participation. Their role in the survey process, if anything, can be even more important and diverse compared to that of the interviewer as they play a role in contact, measurement, obtaining different types of informed consent, and collecting biomeasures. While there is evidence that nurses can have an impact on measurement in biosocial surveys (Cernat and Sakshaug, 2020), their impact on respondent participation has not yet been quantified and there are still many open questions regarding how the effects of nurses vary by country and study, and how they contribute to attrition in longitudinal biosocial studies.
There are at least three stages at which nonresponse can occur during the biomeasure collection phase. The first stage is the decision of the respondent to participate in the biomeasure collection at all. Respondents may refuse the nurse visit entirely, resulting in a complete unit nonresponse for all of the biomeasures (Banks et al., 2006; Kearney et al., 2011; McFall, Conolly, and Burton, 2014). The potential for this type of nonresponse likely increases with the passing of time since the main interview was completed (Watson et al., 2018; Watson and Wooden, 2014). The second stage, conditional on initial participation in the nurse visit, is the decision of the respondent to participate in the collection of each individual biomeasure. This stage usually requires explicit consent from the respondent after they have been informed about how the measurement will be used, stored, and safeguarded. While respondents may consent to the collection of some individual biomeasures, they may refuse to consent to others. Typically, the most invasive measures, such as whole blood collection, yield the lowest consent rates (Jaszczak, Lundeen, and Smith, 2008; Sakshaug, Couper, and Ofstedal, 2010; McFall, Conolly, and Burton, 2014; Weiss, Sakshaug, and Börsch‐Supan, 2019). The third stage of nonresponse occurs when respondents who consent to specific measurements may be unwilling, or physically unable to complete the measurement once it begins. For example, it may not be possible to extract sufficient amounts of blood or saliva from the respondent, or the respondent may experience pain or discomfort during the collection procedure that prevents them from finishing the collection. Equipment issues, mishandled or damaged samples at the shipment or processing stage, or administrator error may also contribute to this form of nonresponse. Typically, this results in the recording of a missing data value in the published dataset.
While longitudinal biosocial surveys are designed to be representative of the target population over time, the multiple stages at which nonresponse can occur during the biological data collection phase can lead to bias in statistical analyses of the collected data (Korbmacher 2014; Sakshaug, Couper, and Ofstedal 2010). In addition, there is no guarantee that respondents who take part in the nurse visit in one wave are willing to do so again in a subsequent wave, particularly when the nurse visit must be scheduled some time after the main interview and invasive biological measures, such as blood, are collected (McFall, Conolly, and Burton, 2014).
One strategy that may be effective in minimizing nonresponse at each stage of the biomeasure collection component over multiple waves of a longitudinal study is nurse continuity; that is, to deploy the same nurse to the same household at each subsequent wave of data collection. While more flexible nurse allocation strategies, such as switching nurses between waves, may be less costly and more convenient to the survey institute, maintaining the continuity of field personnel is generally endorsed by many survey researchers in longitudinal surveys. In the context of traditional interviewer-led surveys, assigning the same interviewer to a previously-interviewed household has been found to reduce subsequent wave nonresponse (Haunberger, 2010; Laurie, Smith, and Scott, 1999; Watson and Wooden, 2014, 2009), though this finding is not universally consistent (Campanelli and O’Muircheartaigh, 2002, 1999; Vassallo et al., 2015) and the effect can be moderated by other factors, such as interviewer experience (Lynn, Kaminska, and Goldstein, 2014). Given the physical burden and potential invasiveness of biomeasure data collection, it is reasonable to postulate that nurse continuity would have a positive effect on respondent participation in the biomeasure component of a biosocial survey. For example, just as medical patients may prefer to visit the same physician over time, respondents in a biosocial survey may feel greater comfort in knowing that the same nurse who collected the biomeasures from them in the previous wave of the study will do so again in the current wave. However, there is virtually no empirical evidence that tests this hypothesis. Thus, the effectiveness of nurse continuity for maximizing participation in all three biomeasure collection stages: 1) nurse visit, 2) biomeasure consent, and 3) the collection of a valid measurement is largely unknown.
While nurse switching can occur for the same reasons as interviewer switching (e.g. scheduling issues, turnover, respondent mobility), it remains to be seen whether the continuity findings reported in the interviewer literature translate to nurses in biosocial surveys. On the one hand, it may be the case that having the same nurse brings a certain level of comfort and familiarity to the respondent which, in turn, leads to steady, or even higher, rates of biomeasure participation. On the other hand, there might be situations where a nurse switch is advantageous for maximizing participation. For example, borrowing again from the interviewer literature, researchers have found that using different interviewers to re-engage previous wave nonrespondents has a positive effect on subsequent wave participation (Watson and Wooden, 2014). It is therefore plausible that switching nurses for respondents who previously didn’t participate in at least one (or all) of the three stages of the biomeasure collection component would have a similar (positive) effect on participation in the subsequent wave. The experience level of the nurse may also play a role. Given the potential complexity of administering the more invasive biomeasures (e.g. blood), switching to a nurse with more experience compared to that of the previous nurse may have positive effects on participation. Conversely, switching from a more experienced nurse to a less experienced nurse would be expected to have potentially adverse effects on participation.
The present study sheds light on these issues by investigating the role of nurse continuity on biomeasure participation in a nationally-representative longitudinal biosocial study of aging, the ELSA. The results of this investigation will inform survey researchers on nurse allocation strategies for maximizing participation in the crucially important biomeasure component of biosocial surveys.
Specifically, this article addresses the following research questions:
- Does nurse continuity increase the likelihood of subsequent wave participation in the biomeasure component of a biosocial survey?
- Does switching nurses increase the likelihood of biomeasure participation among respondents who didn’t participate in the prior-wave biomeasure collection?
- Does switching to a different nurse with more experience compared to the prior-wave nurse positively impact biomeasure participation? Conversely, does switching to a nurse with the same/less experience compared to the prior-wave nurse adversely affect biomeasure participation?
- To what extent, does nurse (dis)continuity differentially impact each stage of the biomeasure collection: participation in the nurse visit, consent to biomeasure collection, and successful biomeasure collection?
2 Data
We study the effects of nurse continuity using the English Longitudinal Study of Ageing (ELSA). ELSA is a panel study that investigates the change in circumstances of older persons (aged 50 years and older) living in England. The data are collected every two years with the baseline wave carried out in 2002. The original sample was selected from respondents of the Health Survey for England (HSE) in years 1998, 1999 and 2001. The HSE is a repeated cross-sectional survey representative of the general population of England (Mindell et al., 2012). Responding households from the HSE were ineligible for ELSA if they had no adult 50 years or older in the household and if they did not agree to be re-contacted. The ELSA data are freely accessible from the UK Data Archive (https://www.data-archive.ac.uk/).
In waves 2, 4, and 6 respondents to the main ELSA interview were invited to take part in a separate nurse visit to collect a variety of biomeasures. Respondents were eligible for the nurse visit if: 1) they were original (or “core”) sample members of the ELSA; 2) were interviewed in-person in the respective wave; 3) didn’t have any clotting/bleeding at the time of the main interview; and 4) had no history of fits or were not taking anticoagulant drugs. Respondents were asked if they were willing to participate in the nurse visit at the end of the main interview. For those who ostensibly agreed to participate in the follow-up nurse visit, they were visited by professional nurses at the respondent’s dwelling several months after the interview. The individual-level response rate in the main ELSA interview for the baseline wave was 67% of those eligible (i.e. HSE responding households from 1998, 1999 and 2001 that had at least one member older than 50 years and agreed to be re-contacted), while for waves 2, 4, and 6 the response rates were 82%, 71% and 76%, respectively, among eligible respondents (Bridges, Hussey, and Blake, 2015; Cheshire et al., 2012; Scholes, Taylor, Cheshire, Cox, and Lessof, 2008; Taylor et al., 2007; for more information about ELSA eligibility criteria, see NatCen Social Research, 2018). Among the survey respondents who ostensibly agreed to the follow-up nurse visit, the response rates for actual participation in the nurse visit at waves 2, 4, and 6 were 87.3%, 85.7% and 84.3%, respectively (NatCen Social Research, 2015).
3 Methods
ELSA is unique in the fact that it has three waves of nurse data collection (waves 2, 4 and 6) from a representative sample, but only the last two waves (waves 4 and 6) are relevant for the present analysis as indicators of nurse switch are not applicable for wave 2. Thus, we analyse nurse visit outcomes in waves 4 and 6 of ELSA where the impact of nurse (dis)continuity is likely to occur. We analyse separately within each wave the response outcomes to three conditional stages: participation in the nurse visit, consent to blood collection, and successful blood collection. We focus on blood collection as this is arguably one of the most important and invasive biomeasures collected in biosocial surveys. We study these three outcomes separately as the participation mechanisms of each one can be different and separating them will better inform each step of the response process and determine any differential impact of nurse continuity.
Given that the participation outcome variables of interest are dichotomous, we estimate probit regression models that transform the original outcome variable using a probit link function (Agresti, 2007). Additionally, the modelling approach accounts for the hierarchical nature of the data as respondents are nested within nurses and geographical areas, namely, Lower Super Output Areas (LSOA). LSOAs are geospatial statistical units which define areas with a minimum population size of 1,000 and a mean size of 1,500. They are used for the reporting of small area statistics in England and Wales.
The geographical component is considered one of the main potential threats to the estimation of nurse (or interviewer effects) due to the lack of a random allocation of nurses in ELSA and the possible correlation with area characteristics (e.g. nurses might receive better training in wealthier areas). For this reason, we incorporate geography into the modelling approach to partially control for this confounding as highlighted by West and Blom (2017).
The multilevel probit cross-classified model is specified as:
![]()
where the outcome of interest, ![]() , varies by
, varies by ![]() individuals,
individuals, ![]() areas, and
areas, and ![]() clusters (the latter two being cross-classified). The outcome is explained by an intercept term,
clusters (the latter two being cross-classified). The outcome is explained by an intercept term, ![]() , and
, and ![]() independent variables. Both areas and nurses have estimated variance components,
independent variables. Both areas and nurses have estimated variance components, ![]() and
and ![]() , respectively. The residual error is fixed to 1 by default and is not estimated.
, respectively. The residual error is fixed to 1 by default and is not estimated.
To estimate the models, Bayesian estimation is implemented in Mplus 8.1 using non-informative priors (Asparouhov and Muthén, 2010). Bayesian estimation provides a framework capable of estimating complex models such as the cross-classified models used here, which overcome some of the limitations of maximum likelihood estimation. Four chains were used with 25,000 iterations and a thinning coefficient of 30. We applied a convergence criterion of 1.01 for the Potential Scale Reduction indicator. Trace plots and posterior distributions were inspected for possible convergence issues.
For each wave and outcome, three models are estimated: 1) the Baseline model, 2) the Main Effects model, and 3) the Extended model. The Baseline model contains only control variables which account for possible confounding both at the respondent and nurse level. The control variables at the respondent level include: gender, having a partner, living alone, being white, age, education, owning their house, living in the North of England, living in London, self-reported health, and lagged outcome variables from the previous-wave nurse visit: if they participated in the nurse visit, if they consented to blood collection, and if the blood collection was successful. Descriptive statistics for each of these variables are available in the appendix. The control variables at the nurse level include: nurse age (in years: <55, 55-64, 65+) and years of experience as a nurse (0-5, 6-10, 11-15, 16+).
The Main Effects model contains all control variables from the baseline model plus indicators of nurse continuity: if the nurse changed compared to the previous wave and, for wave 6, if the respondent had the same nurse at all three nurse visit waves (waves 2, 4, and 6). We also include a missing data category if nurse change information is missing, which occurred for about 7% (wave 4) and 3% (wave 6) of the nurse visits.
The Extended model includes all variables from the previous models plus interactions of nurse change with: 1) nurse experience (more, same, or less compared to the previous-wave nurse); and 2) each lagged outcome of the previous wave nurse visit: nurse visit participation, consent to blood collection, and successful blood collection. The interactions of nurse change in the Extended model allow us to answer research questions two and three. Further, by comparing the Baseline model with the Extended model we estimate the proportion of total variation that is explained by nurse continuity after controlling for potential confounders. This enables us to rank the importance of the nurse continuity indicators for each of the three biomeasure participation outcomes.
4 Results
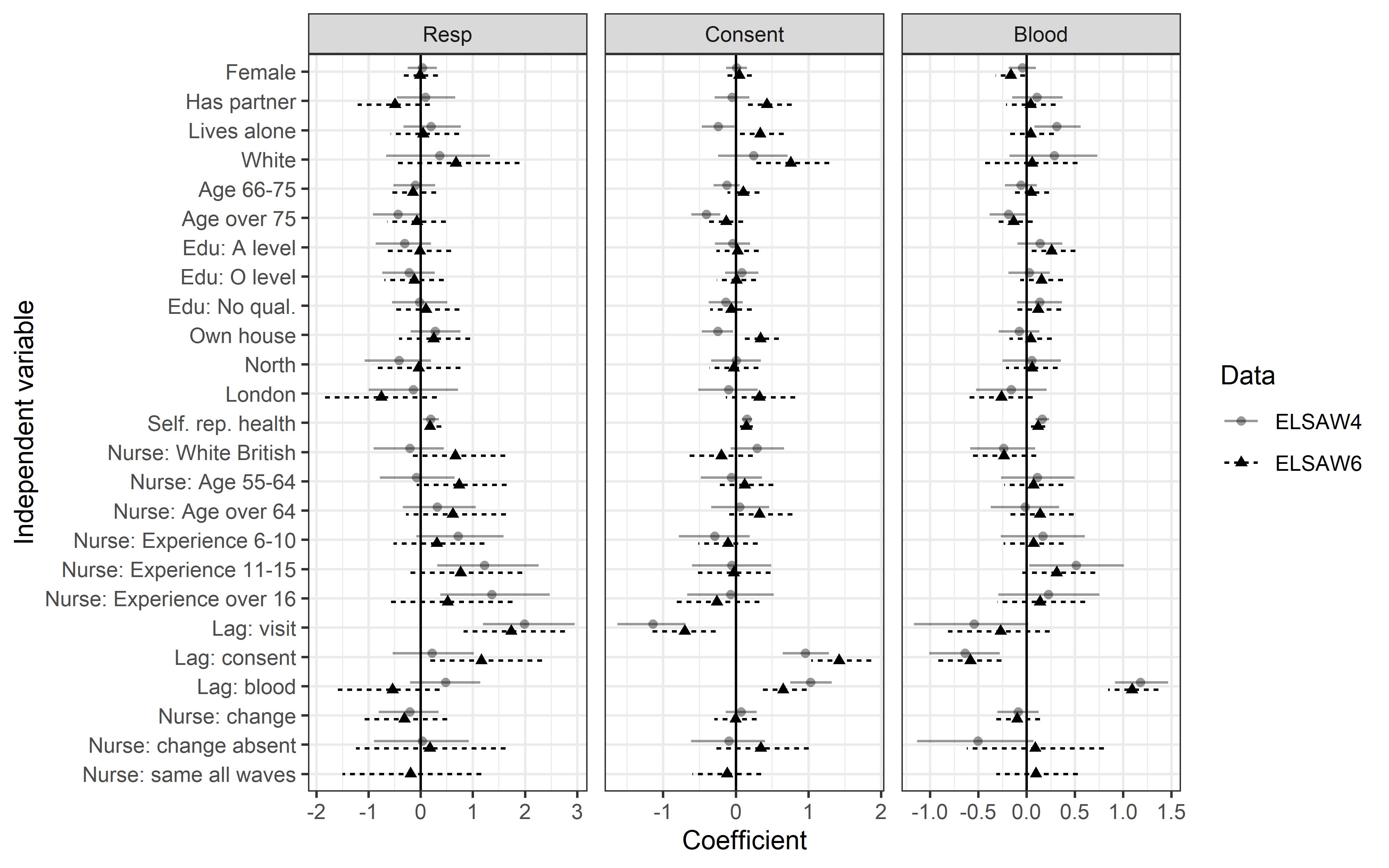
We begin by presenting the Main Effects model that explains participation to each of the three biomeasure participation outcomes: the nurse visit, consent to giving blood, and successful blood collection for waves 4 and 6 of the ELSA. Figure 1 presents the point estimates and the credible intervals (tabular results available upon request). We note that an estimate is considered to be statistically significant if its credible interval does not include zero. The most important predictors of each outcome are their respective lag outcomes at the previous wave. For example, participating in the nurse visit at the previous wave increases the likelihood of participation in waves 4 and 6. This is also true for consent to blood collection and successful blood collection. Another consistent finding is that higher levels of self-rated health lead to higher participation in each of the stages of biomeasure participation. Also of note is that nurses with more experience are more likely to obtain participation to the nurse visit and blood collection in wave 4. On the other hand, nurse’s age does not have a significant impact on participation to any of the biomeasure outcomes in waves 4 and 6 of ELSA.
Looking at the effect of nurse continuity (research question one), it is apparent that switching nurses does not have a significant effect on participation in any of the outcomes or waves. This is also true for the indicator of having the same nurse in all three waves (for the wave 6 outcomes), suggesting that nurse continuity does not significantly impact participation in biomeasure collection.
Fig 1 Main Effects model and credible intervals for three nurse visit outcomes in ELSA waves 4 and 6 estimated using cross-classified probit regression models. Please note the varying x-axis scales for the three dependent variables.
We further develop the model to include interactions between nurse switch and nurse experience and lag outcomes to answer research questions two and three. Looking at the Extended model in Figure 2 (tabular results available upon request) one can see that most often changing the nurse does not have a significant effect on the participation outcomes (i.e. the credible interval includes zero). There are three exceptions. The first exception is the positive effect of nurse change on the likelihood of receiving consent to blood collection in wave 4 for those respondents who did not participate in the previous wave and were attended to by a nurse with the same level of experience (a coefficient estimate of 1.6 on the probit scale). Additionally, in wave 4, changing the nurse when there was a successful lag nurse visit in the previous wave with a nurse that has the same experience level leads to a decrease in the likelihood of getting consent for blood collection (a coefficient estimate of -1.3 on the probit scale). On the other hand, in wave 6 of ELSA, changing the nurse to one with more experience for nonrespondents to the previous wave appears to decrease the chances of nurse visit participation (a coefficient estimate of -1.17 on the probit scale).
Fig 2 Extended Model and credible intervals for three nurse visit outcomes in ELSA waves 4 and 6 estimated using cross-classified probit regression models. Please note the varying x-axis scales for the three dependent variables.
Looking at the proportion of variance explained in the Baseline and Extended models in Table 1, it is apparent that accounting for nurse continuity indicators improves the models and this is especially true for the nurse visit participation outcome where 9% and 13% of the variation is explained in waves 4 and 6, respectively. For consent to blood collection and for successful blood collection the nurse stability variables explain only a small amount of the variation (between 2-3%) across the waves.
Table 1. Percentage of variance explained in each biomeasure outcome by the regression models
| Biomeasure outcome |
Wave |
Baseline model |
Extended model | Difference |
| Visit participation |
4 |
55% |
64% | 9% |
|
6 |
51% | 65% |
13% |
|
| Consent to blood collection |
4 |
35% |
36% | 2% |
|
6 |
39% | 42% |
3% |
|
| Successful blood collection |
4 |
18% |
20% |
2% |
|
6 |
17% | 19% |
2% |
5 Discussion
This study investigated the impact of nurse continuity on respondent participation in the biomeasure component of a nationally-representative longitudinal biosocial survey. Overall, we found that changing nurses from one wave to another or assigning the same nurse to all three waves (2, 4, and 6) of the English Longitudinal Study of Ageing (ELSA) has no significant impact on the likelihood of participating in each of the three stages of the biomeasure collection component (research question one): nurse visit participation, consent to blood collection, and successful blood collection. Looking at how nurse switching interacts with nurse experience and previous wave outcomes (research questions two and three), only a few effects were observed. We found that changing the nurse for nonrespondents to the previous wave with a nurse with the same level of experience in the current wave increases the likelihood of consent to blood collection in wave 4, but changing the nurse for respondents to the previous wave nurse visit with a nurse with the same level of experience has a negative effect on consent to blood collection. In wave 6, we found that switching to a more-experienced nurse for nonrespondents in the previous wave decreases the likelihood of participation in the nurse visit. Lastly, we do not observe large variations between the different participation outcomes in the biomeasure component (research question four). The three statistically significant effects found were related to either nurse visit participation or consent to blood collection, and no impact on the likelihood of successful blood collection was found. We did find, however, that the nurse continuity indicators explained more variation in the nurse visit participation outcome compared to the other biomeasure outcomes (i.e. consent to blood collection and successful blood collection conditional on consent).
The results paint a somewhat reassuring picture for biosocial survey practice. Overall, the potential added expense of maintaining nurse continuity in a longitudinal biosocial study may not be necessary for maximizing biomeasure participation. This finding runs counter to other survey studies which show that continuity of fieldwork personnel (namely, interviewers) tends to have positive effects on longitudinal response rates (Haunberger, 2010; Laurie, Smith, and Scott, 1999; Watson and Wooden, 2014, 2009). However, the finding that switching nurses with the same level of experience for previous wave nonrespondents improves the likelihood of consent to blood collection is consistent with other work which shows that switching interviewers is effective for re-engaging previous-wave survey nonrespondents (Watson and Wooden, 2014). Swapping nurses with similar levels of experience is likely to be a reasonable and cost-effective strategy for survey institutes, assuming that nurse salary bands are commensurate with experience level. On the other hand, switching to a more-experienced nurse for previous-wave nonrespondents could have added costs and may not necessarily improve nurse visit participation, as we observed in the ELSA. More research is needed to explicate this counterintuitive finding.
Like most observational studies, this one has limitations. Firstly, the change of nurses was not experimentally controlled. As such, there is a potential for confounding effects. We addressed this issue by incorporating several control variables, including respondent and nurse characteristics, as well as two random effects for nurses and areas into our modelling approach, but the potential for unobserved confounders could still remain. Additionally, we investigated the effects of nurse continuity in only one study. While the ELSA is widely considered to be a high-quality, nationally-representative survey of England, there could be possible idiosyncrasies related to the country, period, and population covered that might limit the external validity of the results. Similarly, in this study we ignore possible confounding effects of interviewers in the main study and nurse continuity. Lastly, we do not account for the confounding of time in panel (which is linked to interest in the topic and commitment) with the impact of nurses. For this a quasi-experimental design, such as comparisons with refreshment samples would be needed. We encourage more research that addresses these limitations and confirm the generalizability of the findings.
These limitations highlight the fact that there is a need to understand the role of the nurse in the context of the Total Survey Error framework and all the different stages of data collection. Here we only focused on the nurse stage of the survey and in this process have ignored potential confounders such as the impact of interviewers at earlier stages. Other aspects like incentives, the organization carrying out the survey, the timing of the main survey may also be important and interact with our results. Of special importance in this context is the role of the interviewer that can have carry-over effects in the nurse visit, possibly even several months after the main interview. This effect could be larger for some aspects, such as initial participation in the nurse visit, but are probably less relevant for other stages, such as consent and blood data collection, where the skill of the nurse is especially important. Further research is needed to understand the interactions between nurses and interviewers in these complex data collections.
In conclusion this study is the first to investigate how the continuity of nurses in a longitudinal biosocial survey can impact respondent participation in biological data collection. In line with the literature on interviewer continuity, our findings are mixed. Overall, there are no systematic impacts of maintaining nurse continuity in both waves 4 and 6 of ELSA or across the multiple participation outcomes. Nonetheless there are some effects of changing nurses that might improve participation, particularly for respondents who didn’t participate in the previous-wave nurse visit. Based on these findings, we conclude that nurse continuity does not have a strong impact on respondent participation in a longitudinal biosocial survey. Further research is needed to assess the robustness of these findings in other biosocial surveys.
6 Appendix
Table A1. Descriptive statistics of ELSA (waves 4 and 6) variables used in analysis
| Variables | Code | Freq wave 4 | % wave 4 | Freq wave 6 | % wave 6 |
| Nurse response | No | 258 | 4.5 | 214 | 4.4 |
| Yes | 5494 | 95.5 | 4634 | 95.6 | |
| Blood consent | No | 502 | 8.7 | 389 | 8 |
| Yes | 4628 | 80.5 | 3939 | 81.2 | |
| Ineligible | 622 | 10.8 | 520 | 10.7 | |
| Blood collection | No | 334 | 5.8 | 304 | 6.3 |
| Yes | 4294 | 74.7 | 3635 | 75 | |
| Ineligible | 1124 | 19.5 | 909 | 18.8 | |
| Female | No | 2552 | 44.4 | 2151 | 44.4 |
| Yes | 3200 | 55.6 | 2697 | 55.6 | |
| Has partner | No | 1872 | 32.5 | 1634 | 33.7 |
| Yes | 3880 | 67.5 | 3214 | 66.3 | |
| Lives alone | No | 3234 | 56.2 | 2660 | 54.9 |
| Yes | 2518 | 43.8 | 2188 | 45.1 | |
| White | No | 119 | 2.1 | 114 | 2.4 |
| Yes | 5633 | 97.9 | 4734 | 97.6 | |
| Age | 48-65 | 2435 | 42.3 | 1385 | 28.6 |
| 66-75 | 1925 | 33.5 | 1982 | 40.9 | |
| Over 75 | 1392 | 24.2 | 1481 | 30.5 | |
| Edu | Higher | 910 | 15.8 | 766 | 15.8 |
| A level | 1244 | 21.6 | 1072 | 22.1 | |
| O level | 1881 | 32.7 | 1691 | 34.9 | |
| No qual | 1713 | 29.8 | 1294 | 26.7 | |
| Own house | No | 948 | 16.5 | 753 | 15.5 |
| Yes | 4804 | 83.5 | 4095 | 84.5 | |
| North | No | 4119 | 71.6 | 3492 | 72 |
| Yes | 1633 | 28.4 | 1356 | 28 | |
| London | No | 5257 | 91.4 | 4462 | 92 |
| Yes | 495 | 8.6 | 386 | 8 | |
| Self. rep. health | Poor | 405 | 7 | 374 | 7.7 |
| Fair | 1193 | 20.7 | 1049 | 21.6 | |
| Good | 1909 | 33.2 | 1611 | 33.2 | |
| Very good | 1633 | 28.4 | 1363 | 28.1 | |
| Excellent | 612 | 10.6 | 451 | 9.3 | |
| Nurse: White British | No | 1923 | 33.4 | 755 | 15.6 |
| Yes | 3829 | 66.6 | 4093 | 84.4 | |
| Nurse age | Under 54 | 1476 | 25.7 | 1218 | 25.1 |
| 55-64 | 1580 | 27.5 | 2036 | 42 | |
| Over 64 | 2696 | 46.9 | 1594 | 32.9 | |
| Nurse experience | 1-5 | 923 | 16 | 1159 | 23.9 |
| 6-10 | 2202 | 38.3 | 1949 | 40.2 | |
| 11-15 | 1325 | 23 | 943 | 19.5 | |
| Yes | 1302 | 22.6 | 797 | 16.4 | |
| Nurse: same all waves | No | 5429 | 94.4 | 4529 | 93.4 |
| Yes | 323 | 5.6 | 319 | 6.6 | |
| Nurse: change | No | 1616 | 28.1 | 1127 | 23.2 |
| Yes | 4136 | 71.9 | 3721 | 76.8 | |
| Nurse: change absent | No | 5371 | 93.4 | 4725 | 97.5 |
| Yes | 381 | 6.6 | 123 | 2.5 | |
| Lag: visit | No | 536 | 9.3 | 271 | 5.6 |
| Yes | 5216 | 90.7 | 4577 | 94.4 | |
| Lag: consent | No | 1105 | 19.2 | 863 | 17.8 |
| Yes | 4647 | 80.8 | 3985 | 82.2 | |
| Lag: blood | No | 1373 | 23.9 | 1145 | 23.6 |
| Yes | 4379 | 76.1 | 3703 | 76.4 |
References
- Agresti, A. (2007). An Introduction to Categorical Data Analysis (2nd Revised edition edition). Hoboken, NJ: John Wiley & Sons.
- Asparouhov, T., & Muthén, B. (2010). Bayesian Analysis Using Mplus: Technical Implementation. Mplus.
- Banks, J., Breeze, E., Lessof, C., and Nazroo, J. (2006). Retirement, health and relationships of the older population in England: The 2004 English Longitudinal Study of Ageing (Wave 2). Institute for Fiscal Studies.
- Beebe, T. J. (2007). Challenges of Collecting Survey-Based Biomarker and Genetic Data. Proceedings of the 9th Conference on Health Survey Research Methods. Peachtree City, GA; 2007.
- Bridges, S., Hussey, D., and Blake, M. (2015). The dynamics of ageing: The 2012 English Longitudinal Study of Ageing (Wave 6) [Technical Report]. NatCen.
- Campanelli, P., and O’Muircheartaigh, C. (1999). Interviewers, interviewer continuity, and panel survey nonresponse. Quality and Quantity, 33(1), 59–76.
- Campanelli, P., and O’Muircheartaigh, C. (2002). The importance of experimental control in testing the impact of interviewer continuity on panel survey nonresponse. Quality and Quantity, 36(2), 129–144.
- Cernat, A., and Sakshaug, J.W. (2020). Nurse effects on measurement error in household biosocial surveys. BMC Medical Research Methodology, 20:45.
- Cheshire, H., Hussey, D., Medina, J., Piekering, K., Wood, N., Ward, K., Taylor, K., and Lessof, C. (2012). Financial circumstances, health and well-being of the older population in England: The 2008 English Longitudinal Study of Ageing [Technical series].
- Das, A. (2013). How does race get “under the skin”?: Inflammation, weathering, and metabolic problems in late life. Social Science & Medicine, 77, 75–83.
- Das, A. (2019). Loneliness does (not) have cardiometabolic effects: A longitudinal study of older adults in two countries. Social Science & Medicine, 223, 104–112.
- Das, A., and Nairn, S. (2014). Religious attendance and physiological problems in late life. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 71(2), 291–308.
- Geronimus, A. T., Pearson, J. A., Linnenbringer, E., Schulz, A. J., Reyes, A. G., Epel, E. S., Lin, J., and Blackburn, E. H. (2015). Race-ethnicity, poverty, urban stressors, and telomere length in a Detroit community-based sample. Journal of Health and Social Behavior, 56(2), 199–224.
- Haunberger, S. (2010). The effects of interviewer, respondent and area characteristics on cooperation in panel surveys: A multilevel approach. Quality & Quantity, 44(5), 957–969.
- Holmes, L. M., and Marcelli, E. A. (2012). Neighborhoods and systemic inflammation: High CRP among legal and unauthorized Brazilian migrants. Health & Place, 18(3), 683–693.
- Honda, T., Pun, V. C., Manjourides, J., and Suh, H. (2017). Associations between long-term exposure to air pollution, glycosylated hemoglobin and diabetes. International Journal of Hygiene and Environmental Health, 220(7), 1124–1132.
- Jaszczak, A., Lundeen, K., and Smith, S. (2008). Using Nonmedically Trained Interviewers to Collect Biomeasures in a National In-home Survey. Field Methods, 21(1), 26–48.
- Kearney, P. M., Cronin, H., O’Regan, C., Kamiya, Y., Savva, G. M., Whelan, B., and Kenny, R. (2011). Cohort profile: The Irish Longitudinal Study on Ageing. International Journal of Epidemiology, 40(4), 877–884.
- Korbmacher, J. M. (2014). Interviewer Effects on Respondents’ Willingness to Provide Blood Samples in SHARE. SHARE Working Paper Series 20.
- Laurie, H., Smith, R. A., and Scott, L. (1999). Strategies for reducing nonresponse in a longitudinal panel survey. Journal of Official Statistics, 15(2), 269–282.
- Ludwig, J., Sanbonmatsu, L., Gennetian, L., Adam, E., Duncan, G. J., Katz, L. F., Kessler, R. C., Kling, J. R., Lindau, S. T., and Whitaker, R. C. (2011). Neighborhoods, obesity, and diabetes—A randomized social experiment. New England Journal of Medicine, 365(16), 1509–1519.
- Lynn, P., Kaminska, O., and Goldstein, H. (2014). Panel attrition: How important is interviewer continuity? Journal of Official Statistics 30, 443-457.
- McFall, S. L., Booker, C., Burton, J., and Conolly, A. (2012). Implementing the biosocial component of Understanding Society–Nurse collection of biomeasures. Institute for Social and Economic Research, University of Essex.
- McFall, S. L., Conolly, A., and Burton, J. (2014). Collecting Biomarkers Using Trained Interviewers. Lessons Learned from a Pilot Study. Survey Research Methods, 8(1), 57–66.
- Mindell, J., Biddulph, J. P., Hirani, V., Stamatakis, E., Craig, R., Nunn, S., and Shelton, N. (2012). Cohort Profile: The Health Survey for England. International Journal of Epidemiology, 41(6), 1585–1593.
- NatCen Social Research. (2015). English Longitudinal Study of Ageing (ELSA) Wave 2, 4 and 6 User Guide to the nurse datasets. NatCen Social Research, London, England.
- NatCen Social Research. (2018). User Guide to the Main Interview Datasets. NatCen Social Research, London, England.
- National Research Council. (2000). Cells and Surveys: Should Biological Measures Be Included in Social Science Research? The National Academies Press: Washington, DC
- National Research Council. (2007). Biosocial Surveys. The National Academies Press: Washington, DC
- National Research Council. (2010). Conducting Biosocial Surveys: Collecting, Storing, Accessing, and Protecting Biospecimens and Biodata. The National Academies Press: Washington, DC
- Sakshaug, J. W., Couper, M. P., and Ofstedal, M. B. (2010). Characteristics of physical measurement consent in a population-based survey of older adults. Medical Care, 48(1), 64–71.
- Sakshaug, J. W., Ofstedal, M. B., Guyer, H., and Beebe, T. J. (2015). The Collection of Biospecimens in Health Surveys. In: T. Johnson (Ed.). Handbook of Health Survey Methods. Hoboken, NJ: John Wiley and Sons, pp. 383-419.
- Scholes, S., Taylor, R., Cheshire, H., Cox, K., and Lessof, C. (2008). Retirement, health and relationships of the older population in England: The 2004 English Longitudinal Study of Ageing [Technical series].
- Steptoe, A., Breeze, E., Banks, J., and Nazroo, J. (2013). Cohort Profile: The English Longitudinal Study of Ageing. International Journal of Epidemiology, 42(6), 1640–1648.
- Taylor, R., Conway, L., Calderwood, L., Lessof, C., Cheshire, H., Cox, K., and Scholes, S. (2007). Health, wealth and lifestyles of the older population in England: The 2002 English Longitudinal Study of Ageing [Technical series].
- Vassallo, R., Durrant, G. B., Smith, P. W., and Goldstein, H. (2015). Interviewer effects on non-response propensity in longitudinal surveys: A multilevel modelling approach. Journal of the Royal Statistical Society: Series A (Statistics in Society), 178(1), 83–99.
- Watson, N., Leissou, E., Guyer, H., and Wooden, M. (2018). Best practices for panel maintenance and retention. In: T. Johnson, B.-E. Pennell, I. Stoop, and B. Dorer (Eds.). Advances in Comparative Survey Methods: Multinational, Multiregional, and Multicultural Contexts (3MC). John Wiley and Sons, pp. 597–622.
- Watson, N., and Wooden, M. (2009). Identifying factors affecting longitudinal survey response. In: P. Lynn (ed.), Methodology of Longitudinal Surveys. Chichester, UK: John Wiley and Sons, pp. 157–182.
- Watson, N., and Wooden, M. (2014). Re-engaging with survey non-respondents: Evidence from three household panels. Journal of the Royal Statistical Society: Series A (Statistics in Society), 177(2), 499–522.
- Weiss, L.M., Sakshaug, J.W., and Börsch-Supan, A. (2019). Collection of Biomeasures in a Cross-National Setting: Experiences in SHARE. In: T. Johnson, B.-E. Pennell, I. Stoop, and B. Dorer (Eds.). Advances in Comparative Survey Methods: Multinational, Multiregional and Multicultural Contexts (3MC). John Wiley and Sons, pp. 623-641.
- West, B.T., and Blom, A.G. (2017). Explaining interviewer effects: a research synthesis. Journal of Survey Statistics and Methodology, 5(2), 175-211.
- Yang, Y. C., Boen, C., Gerken, K., Li, T., Schorpp, K., and Harris, K. M. (2016). Social relationships and physiological determinants of longevity across the human life span. Proceedings of the National Academy of Sciences, 113(3), 578–583.
- Yang, Y. C., Gerken, K., Schorpp, K., Boen, C., and Harris, K. M. (2017). Early-life socioeconomic status and adult physiological functioning: A life course examination of biosocial mechanisms. Biodemography and Social Biology, 63(2), 87–103.